Irritable Bowel Syndrome (IBS) affects millions of people worldwide, causing digestive discomfort and impacting daily life.
Recent research has highlighted the crucial role of the gut microbiome in managing IBS symptoms.
Understanding this relationship can provide valuable insights and actionable tips for those following a low FODMAP diet to alleviate their IBS symptoms.
The gut microbiome consists of trillions of microorganisms, including bacteria, viruses, and fungi, that reside in the digestive tract.
These microorganisms play a vital role in digestion, immunity, and overall health.
An imbalance in the gut microbiome has been linked to various gastrointestinal disorders, including IBS (Shukla & Ghoshal, 2018).
Studies have shown that individuals with IBS often have a different composition of gut bacteria compared to those without the condition.
This dysbiosis can lead to increased intestinal permeability, inflammation, and altered gut motility, all of which contribute to IBS symptoms such as bloating, gas, abdominal pain, and altered bowel habits (Paduano & Cingolani, 2020).
The low FODMAP diet, developed by researchers at Monash University, involves reducing the intake of fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs).
These short-chain carbohydrates are poorly absorbed in the small intestine and can be fermented by gut bacteria, leading to IBS symptoms (Barrett et al., 2013).
While the low FODMAP diet effectively reduces IBS symptoms in many individuals, there are concerns about its long-term impact on the gut microbiome.
Some studies suggest that the diet may reduce beneficial bacteria, such as Bifidobacteria, due to the restricted intake of prebiotic fibres (Staudacher et al., 2014).
The gut microbiome plays a crucial role in IBS, and the low FODMAP diet can help manage symptoms effectively.
By understanding the relationship between gut bacteria and IBS, and incorporating gut-friendly practices, individuals can achieve better digestive health and overall well-being.
References
Barrett, J. S., Gearry, R. B., Muir, J. G., & Gibson, P. R. (2013). Dietary poorly absorbed, short-chain carbohydrates increase delivery of water and fermentable substrates to the proximal colon. Alimentary Pharmacology & Therapeutics, 36(5), 395-407.
Paduano, D., & Cingolani, A. (2020). Alterations of the gut microbiome in irritable bowel syndrome: Still an ongoing debate. Neurogastroenterology & Motility, 32(12), e13931.
Shukla, R., & Ghoshal, U. C. (2018). Gut microbiome and IBS: The evidence is here to stay. World Journal of Gastroenterology, 24(35), 3778-3790.Staudacher, H. M., Lomer, M. C., Farquharson, F. M., & Lindsay, J. O. (2014). Gut microbiota in individuals with irritable bowel syndrome following a low FODMAP diet. Gut, 63(12), 1913-1920.
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols! They are a group of carbohydrates and sugar alcohols found in various foods. Sound confusing? Let’s elaborate.
These compounds are not fully absorbed in the small intestine and instead travel to the large intestine, where they can cause trouble for sensitive tummies, leading to those unwelcome digestive symptoms [1].
Let's meet the members of the different FODMAP groups and common foods which fall within these groups:
Oligosaccharides: These include fructans and GOS (Galacto-Oligosaccharides) and are commonly found in wheat, rye, onions, garlic, and legumes [1].
Disaccharides: Lactose, the sugar present in dairy products such as milk, yogurt, and cheese, falls into this category.
For those with lactose intolerance, consuming these foods can lead to unpleasant symptoms, commonly loose bowel movements [1].
Monosaccharides: Fructose, the natural sugar found in fruits, honey, and high-fructose corn syrup, is part of this group.
While fruits are healthy options, some individuals may experience gut symptoms after eating certain high-fructose fruits [1].
Polyols: These are sugar alcohols like sorbitol, mannitol, xylitol, and maltitol, which can be found in sugar-free gum, stone fruits, and certain artificial sweeteners [1].
These could be the sneaky additions to your diet that contribute to your symptoms of bloating!
Let's discuss the low FODMAP diet approach.
A common myth is that the low FODMAP diet is something you must maintain or stick to in order to maintain your symptoms. This is totally incorrect!
The low FODMAP diet is a 3-step process, not a life-long diet. It's not about banning all FODMAPs forever, because this would actually be terrible for your gut health long-term.
Although they can be problematic to sensitive tummies, These FODMAPs actually provide an essential food source to the healthy bacteria living in your gut, so cutting them out for long periods of time can actually do more harm than good!
Rather we use this low FODMAP diet approach to eliminate these FODMAPs temporarily and then re-introduce each of them to identify your personal food triggers in order to expand your diet again. It involves reducing high FODMAP foods for 4-6 weeks, followed by systematically reintroducing them to determine your triggers and tolerance levels [2].
Remember, it's a 3-step approach, and you don't have to face it alone. Consulting with a registered FODMAP Dietitian can provide valuable guidance and support throughout the process.
Following a low FODMAP diet doesn't mean giving up on delicious meals.
It's all about making smart swaps and exploring FODMAP-friendly options. Seeing your registered FODMAP Dietitian can make the process a lot smoother by providing FODMAP-friendly recipes and meal plans.
Here are some quick tips on what foods to choose on the low FODMAP diet, phase 1:
Please note, this is just a very small glimpse of what you can consume on the low FODMAP diet and you should always consult your local doctor or FODMAP Dietitian before starting the low FODMAP diet.
Remember, taking care of your gut health and overall well-being goes beyond the food you eat.
Managing stress, practising relaxation techniques like yoga or meditation, getting enough sleep, and staying physically active can all contribute to a healthier gut [4]. So, pamper yourself, find activities that bring you joy, and let your inner glow shine.
Remember, the low FODMAP diet should never be undertaken without guidance from a trained professional. For more questions and direction around FODMAPs and the low FODMAP diet, see your doctor or registered FODMAP Dietitian!
[1] Monash University. (n.d.). About FODMAPs. Retrieved from https://www.monashfodmap.com/about-fodmap-and-ibs/
[2] Gibson, P. R., & Shepherd, S. J. (2010). Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach. Journal of Gastroenterology and Hepatology, 25(2), 252-258. doi: 10.1111/j.1440-1746.2009.06149.x
[3] Monash University. (n.d.). Vegetables, Proteins, Grains, Fruits, Sweeteners. Retrieved from https://www.monashfodmap.com/blog/vegetables/
[4] Halmos, E. P., Power, V. A., Shepherd, S. J., Gibson, P. R., & Muir, J. G. (2014). A diet low in FODMAPs reduces symptoms in patients with irritable bowel syndrome and a probiotic restores Bifidobacterium species: a randomized controlled trial. Gastroenterology, 146(1), 67-75. doi: 10.1053/j.gastro.2013.09.046

While IBS is a chronic condition and may never truly resolve, there are several prevention strategies that individuals can implement to manage their symptoms effectively and live with IBS relatively freely.
Here are some strategies that may help prevent IBS flare-ups.
The first step in preventing IBS flare-ups is to identify your personal triggers. If you have not done this, it is time to see a specialist Dietitian and take this first step to finding relief: click here!
FODMAPs are certain types of carbohydrates that are poorly absorbed in the small intestine, leading to symptoms like bloating, abdominal pain, and diarrhea in people with IBS.
Following a low-FODMAP diet can help reduce IBS symptoms, but this should only be followed for a maximum of 6 weeks unless otherwise directed by your Dietitian. It is recommended to work with a specialist dietitian to go through the low FODMAP process. Click here for our recommended specialist Dietitian.
Eating smaller, more frequent meals, chewing food thoroughly, and avoiding trigger foods can help reduce the risk of IBS symptoms flaring up.
Stress management techniques such as deep breathing, meditation, and yoga can help reduce stress levels and prevent IBS flare-ups.
Regular exercise is also an effective stress management tool that can help improve digestion and prevent constipation.
Low intensity exercise can help improve digestion and prevent constipation. Walking, jogging, swimming, and cycling are all effective forms of exercise.
If you're taking medications that are causing IBS symptoms, talk to your Doctor or Dietitian about switching to a different medication or adjusting your dosage.
In some cases, medications may be necessary to manage symptoms.
IBS flare-ups can be very uncomfortable, but with the help of a specialist dietitian to identify triggers and implement prevention strategies, we can help manage your symptoms effectively.
If you want to learn more about how to resolve your IBS symptoms for good, identify your triggers and rebuild a healthy gut, visit @theibsprogram for more information!
The IBS Program is a unique program with a proven framework designed to get you relief for your IBS symptoms as fast and as effectively as possible.

Author: Ellen Kessling, Accredited Practicing Dietitian, IBS & FODMAP Specialist
Ellen is an Accredited Practicing Dietitian & Nutritionist specialising in women’s health, gastrointestinal health and the treatment of irritable bowel syndrome.
Ellen completed her 4-year Health Science Degree at the University of Adelaide, and then went on to complete her 2-year Master's degree in Nutrition & Dietetics at Flinders University. She is a trained Monash FODMAP Dietitian and has developed expertise in gut health and IBS management, and enjoys the area of women’s health, including skin, hormones, fertility, and pre & post pregnancy nutrition.
She loves treating all areas of women's health with a holistic and empathetic approach to practice and encourages sustainable, long-term changes rather than quick fixes. She has a focus on packages and programs in her practice to provide more ongoing, specialised care and support beyond what a 1:1 consultation can offer.
She believes a well-rounded, holistic approach to care leads to more effective and sustainable results in her clients.
By Lisa Kunstler: Nutritionist at FodShop, Personal Trainer, and Group Fitness Instructor
The festive season is a busy time of year with added stresses for those of us with irritable bowel syndrome (IBS) and other dietary conditions. To make sure this season is fun and tummy safe for you and the family, FodShop have collated some tips to enjoy Christmas low FODMAP!

A great idea for low FODMAP Christmas preparations is to bring your own low FODMAP dishes. With Christmas being a busy time of year, our family and friends love the help catering!
You could create a tummy friendly, low FODMAP salad, frittata, or charcuterie board that everyone can enjoy.
Plain, lean meats, parsnips, carrots, potatoes, gluten free crackers, and hard cheeses are some great low FODMAP options.
For some great low FODMAP Christmas food products, like puddings, custard, and gravy, check out the FodShop website HERE.
Low FODMAP diets are often void of fibre, an important component of nutrition found in vegetables, fruits, and wholegrains, that can aid in the prevention of constipation and diarrhoea and decrease abdominal pain. (1)
Approaching Christmas, it is important to keep up your fibre intake and set yourself up for success.
If you’re struggling to consume the recommended 25-30g of fibre per day, try a fibre supplement, like SunFibre or Regular Girl, that may help improve IBS symptoms.
It’s important to start the day right and stay hydrated to prepare your gut for the day.
Manage any concerns or stress you have over the day by meditating, lightly exercising, or chatting to a friend. (2) All of these are great ways to heal the connection between gut and brain and improve IBS symptoms.
Up until the big event, try to avoid FODMAP stacking.
This involves minimising the number of high FODMAP meals consumed during the day to avoid any possible flare ups at Christmas dinner. For more information on FODMAP stacking, check out the recent webinar recording by FodShop and the Diet vs Disease team.
Communication is key on the day to make sure everything runs smoothly.
Try to eat low FODMAP and don’t be afraid to ask for dishes’ ingredients.
Make sure to also limit alcohol and caffeine intake, as both can exacerbate IBS symptoms by irritating the gut. A great alternative is an herbal tea!
If all else fails, there are a variety of enzymatic supplements available at FodShop to get you through the festive season.
Supplements we recommend to IBS patients are Intoleran and FODZYME. Both break down complex FODMAPs, like fructans and lactose, into simple sugars that are easily digestible, making Christmas dinners stress free!
Finally (and most importantly) enjoy and have a Merry low FODMAP Christmas!
About the Author
Lisa Kunstler
Expert Contributor
Email: nutritioninanutshell101@gmail.com
Qualifications: Bachelor of Nutrition Science, Certificate IV in Personal Training, Certificate III in Group Fitness
About: Lisa Kunstler graduated as a Nutritionist from Deakin University in 2022 and has her Certificate III and IV in group fitness and personal training. She has worked at FodShop, a company selling low FODMAP food products for people with irritable bowel syndrome and other conditions, for almost a year. Lisa worked as a student during her degree at the Olive Wellness Institute, where her role involved educating health care professionals on the health benefits of extra virgin olive oil and olive products.
Research/Areas of Interest: Nutrition, Irritable Bowel Syndrome, Fitness, Low FODMAP Diet, the Mediterranean Diet, and the health benefits of Extra Virgin Olive Oil.
For more low FODMAP Recipes check out our Recipe Ebooks! Or download our FREE 4-Day Low FODMAP Meal Plan by entering your email below.
FODMAP stacking could be the reason why your low FODMAP diet is still causing you symptoms. It can occur when you are not paying attention to the amounts of food you are eating along with the types of foods.
FODMAPs are fermentable components of certain carbohydrates found in the food we eat. They are incredibly beneficial to the health of our gut, but in some people, they can cause digestive discomfort and symptoms.
Learn more about what FODMAPs are here.
As the name suggests, it means to eating the same foods high in certain FODMAPs at once in a meal, or across a day.
Usually, on the low FODMAP diet, consuming small amounts of many different foods will not provoke too many symptoms, because it is assumed there is only a small FODMAP content in each small amount of food.
As soon as we increase either the amount of food, or certain types of food, or both, this can cause stacking of FODMAPs.
For example, refer to the diagram below as you read the following scenario; if we choose many high-fructan foods in one meal, even though they may be low FODMAP individually, they become stacked. This means, many small amounts of FODMAPs equal a larger amount of FODMAPs. This may then exceed your symptom threshold and provoke symptoms.
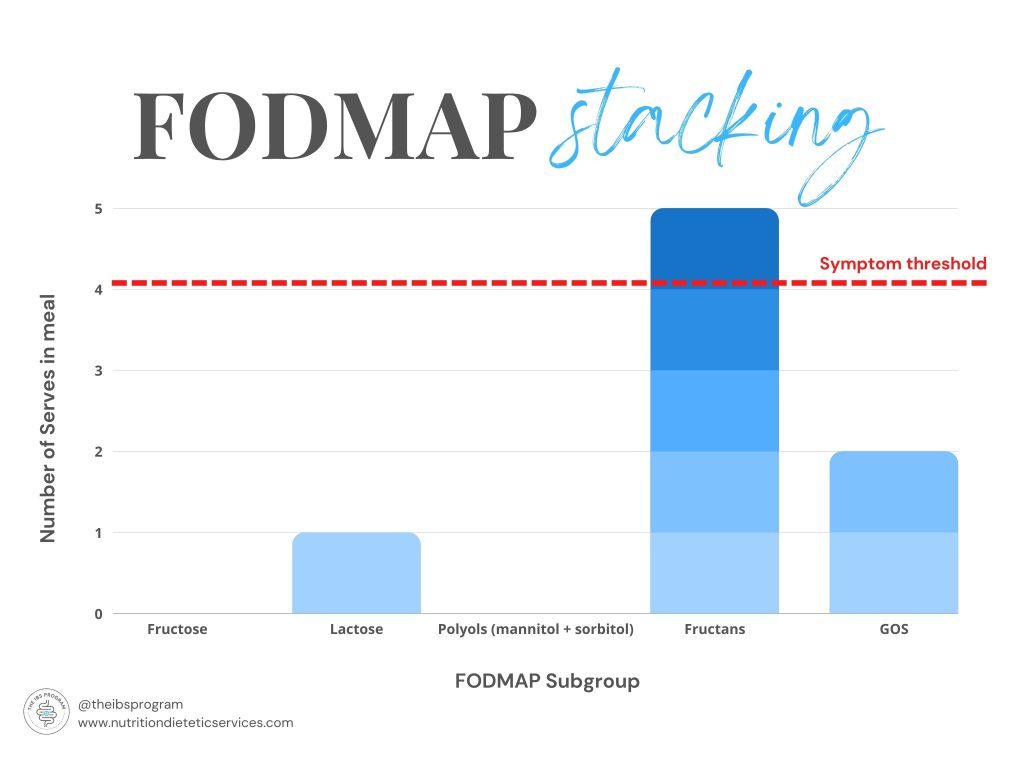
For the everyday person without gut discomfort, this is not a problem at all.
However, those who suffer from IBS generally have a symptom ‘threshold’ whereby they do not experience symptoms when they consume a certain load of each FODMAP in a meal, or across a day.
Stacking FODMAPs means a meal low in FODMAPs can still exceed that threshold and therefore cause symptoms.
See our 7-day low FODMAP meal plan, or 50 low FODMAP snack recipes.
Look at your meal against the FODMAP subgroups and assess whether your meal is particularly high in a certain FODMAP.
If it is dominant in one particular FODMAP, try to remove certain things from your meal or reduce the amount of each component and increase other parts of the meal instead.
If you need help undergoing the low FODMAP diet properly with support, or learning more about FODMAP stacking in your personal situation, book an appointment with our Dietitian who specialises in IBS and the low FODMAP diet, or join The IBS Program.
8 low FODMAP diet swaps for your every day cooking.
Swap some of those high FODMAP foods to a low FODMAP alternative to reduce symptoms of bloating, abdominal pain, excessive gas, and irregular bowel movements.
Garlic chives and garlic-infused oil are the most obvious swaps for a low FODMAP alternative.
The FODMAPs in garlic are actually water-based, therefore they will not contaminate the oil when infused in the liquid so it is safe to consume this as a low FODMAP flavour.
Cobram Estate offer a range of infused oils to help flavour your meals without the use of garlic and onion.
Lactose and products high in lactose are considered high FODMAP, therefore regular yogurt fits in this category.
Choosing preferably a dairy-free yogurt is a great alternative as it has more nutritional value than coconut yogurt. However, coconut yogurt is still a low FODMAP alternative to yogurt.
Wholegrains are extremely beneficial for our health, so we should be careful about which ones we limit on a low FODMAP diet.
Unfortunately, wheat contains fructans which can be problematic on a low FODMAP diet. Instead of choosing regular bread, gluten-free varieties are better tolerated for the short period of time you are on the low FODMAP diet.
Alternatively, some people tolerate rye sourdough much better than regular bread so this is also worth a try.
One of the hardest things to cut out on a low FODMAP diet can be those snack foods, chips, biscuits, dips. But – you don’t actually have to!
There are many low FODMAP biscuit and cracker varieties on the market now days, such as:
For more low FODMAP snacks, check out our 50 low FODMAP snack recipes.
Similar to the onion-infused oil as listed above, there are low FODMAP alternatives to choose from. Onion can be substituted with things such as chives, thyme and other herbs, and the green portion of spring onion. For more flavour options for cooking, visit FodShop.
Regular pasta is referring to white or wholemeal pasta varieties. Pasta is considered a high FODMAP food due to the fructans in the wheat which forms the pasta. Low FODMAP pasta varieties are available, we just have to look for those that are not made from wheat or other grain alternatives.
Low FODMAP pasta options include gluten-free pasta varieties, vermicelli noodles and soba noodles.
Be careful when choosing ‘gluten free’ pasta options, and avoid options that are made out of the following:
All other gluten free options should be suitable on a low FODMAP diet. If ever unsure, please contact us.
Soft drinks and other carbonated drinks such as energy drinks, diet sodas, even soda water can contribute to symptoms of bloating, excessive gas and pain in IBS.
When we consume carbonated drinks, the air within these drinks cannot be reabsorbed in the body, therefore it travels through our system to our large intestine where it can be trapped as gas, contribute to bloating or pass as flatulence.
Avoid all carbonated drinks and soft drinks on the low FODMAP diet.
Instead, try small amounts of regular cordial as a sweet low FODMAP alternative.
A lot of people with IBS suffer from symptoms of bloating, gas and diarrhoea when consuming excess amounts of wine and beer. This is a normal reaction for those with IBS.
To reduce the effect of alcohol on IBS, we can choose different alcoholic options.
Obviously, minimising alcohol is going to benefit symptoms of IBS, but we can also choose other varieties of alcohol that are less symptom-causing.
Spirits are a less symptom-causing alcoholic choice if you have IBS. Be mindful, the mixer paired with the alcohol can also contribute to symptoms, so if you are pairing a carbonated drink such as coke or soda water this can still be problematic for your IBS.
Gluten-free beer options may also be less symptom-causing on IBS symptoms.
Follow @theibsprogram on Instagram for recipes and more food swaps.
For more Low FODMAP recipes, download our FREE Low FODMAP Meal Plan.
Before explaining what the low FODMAP diet is, there are a few things that most people don't know before starting the low FODMAP diet.
See The IBS Program for more information on how to undergo the low FODMAP diet properly and resolve your symptoms of Irritable Bowel Syndrome.
The low FODMAP diet is a 3 phased diet, designed for those with Irritable Bowel Syndrome to help reduce and manage their symptoms.
The low FODMAP diet is designed to reduce the consumption of certain foods called fermentable carbohydrates or FODMAPs, which can lead to symptoms in those with Irritable Bowel Syndrome (IBS).

Certain foods are fermentable carbohydrates (FODMAPs) which can undergo different processes during digestion, causing symptoms such as bloating, gas, urgency, abdominal pain, discomfort and varied bowel habits such as constipation and diarrhoea, or a combination of both.
If you have been diagnosed with Irritable Bowel Syndrome, please book an appointment with a Dietitian to undergo The IBS Program and manage your symptoms within just a few weeks.
If you suspect you may suffer from Irritable Bowel Syndrome, please book an appointment to consult with a qualified Dietitian.
When you receive a diagnosis for Irritable Bowel Syndrome from your doctor or Gastroenterologist it is then suitable for you to consult with a Dietitian about undergoing the low FODMAP diet.
If you are experiencing symptoms and are unsure if you may have it, a Dietitian can help to guide you with what to do next.
Book an online appointment with a qualified Dietitian here.
For those suffering with Irritable Bowel Syndrome, the low FODMAP diet provides a variety of foods that are less fermentable and hence less symptoms causing for those suffering with Irritable Bowel Syndrome.
The low FODMAP diet is not a lifelong diet.
It is important that you undergo the low FODMAP diet under the supervision of a qualified Dietitian trained in the area. The complete low FODMAP diet process looks different for every individual, but the maximum amount of time on the low FODMAP diet should only be 8-12 weeks unless otherwise specified by your Dietitian.
If you are suffering from symptoms of bloating, excessive gas, discomfort, abdominal pain, urgency, or varied bowel habits ranging from constipation to diarrhoea, please see The IBS Program to gain relief from your IBS.
Download our FREE Low FODMAP Meal Plan below.
FODMAPs are fermentable components of certain carbohydrates found in the food we eat. They are incredibly beneficial to the health of our gut, but in some people, they can cause digestive discomfort and symptoms.
Read more to find out what is FODMAP...
FODMAP stands for Fermentable, Oligosaccharides, Disaccharides, Monosaccharides and Polyols.
Those who suffer from Irritable Bowel Syndrome (IBS) will feel the effects of high FODMAP consumption.
These fermentable carbohydrates cause symptoms such as bloating, gas, urgency, abdominal pain, discomfort and varied bowel habits such as constipation and diarrhoea or a combination of both when consumed in the wrong combinations, or amounts.
The presence of these carbohydrates in the digestive system can cause water to be dragged into the small intestine, leading to bloating and diarrhoea. Also, because they aren’t readily absorbed in the small intestine, they can travel into the large intestine where the bacteria ferment them, producing gas as a by product. This gas can lead to bloating, and expansion of the gut, causing pain in those with IBS.
People with IBS have highly sensitive intestines, meaning they may produce similar amounts of gas as someone without IBS, but they feel the effects of it.
There are different subgroups of foods that sit underneath these FODMAP categories and people with IBS may react to 1 or more of these subgroups.
To reduce FODMAP load in your diet and alleviate these symptoms, consult our Dietitian about trailing the diet, or take a look at The IBS Program and undergo the low FODMAP diet independently or with additional support.
The Low FODMAP diet was developed as a tool to help people with IBS manage their diet and alleviate symptoms. If you need help with low FODMAP recipes, download our free meal plan below!
Follow @theibsprogram on Instagram for daily tips and tricks on the low FODMAP diet.